I had so many strange questions before I got my tubal salpingectomy and I discussed them pretty openly with the people around me.
One night over the holidays I was sitting with my partner and my dad at a bar and were all talking about how interesting and unusual it was.
“So they take out the whole tube?”
“Yes, the whole tube. No fallopian tubes.”
“Where do… the eggs go?”
“Probably just like, into your body? They’re really small.”
“No, that can’t be right.”
Turns out, it was right. Your body does keep producing ova after the procedure, and they just kind of get spit out and dissolve.
All the annoying things people who don’t want kids have ever heard. Post continues after.
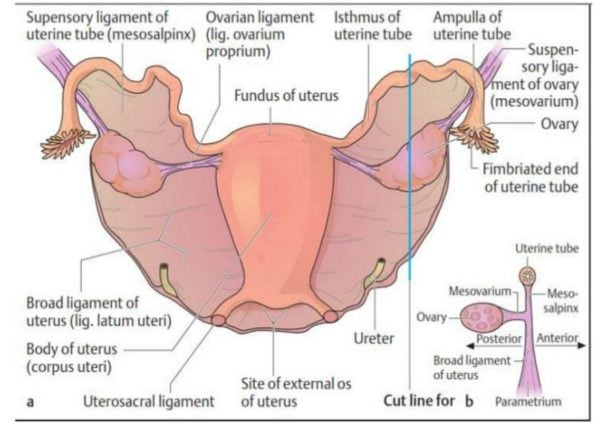
Over the month between when I finally got approval for elective sterilisation and when I actually had the procedure done, I learned more about my reproductive organs than in any sex ed class or My Body, My Self-esque book.