When babies when they're born, they are required to get a heel prick test to check for a number of various genetic diseases. When Rachelle took her son Wade to get his, she didn't expect too much from it.
Then six weeks later, she received a call saying there was a chance Wade had cystic fibrosis. And after further testing, the diagnosis was confirmed.
"There was a lot of grief [when we first found out]," Rachelle tells Mamamia.
"There was grief that he would be taken away before he got to fulfil his purpose. There was a selfish grief as well for our family, knowing we would have to make a lot of sacrifices. It was overwhelming."
For Rachelle, who is a paramedic, she had some background knowledge on what cystic fibrosis (CF) is. But it was nothing compared to the lived experience her family has now.
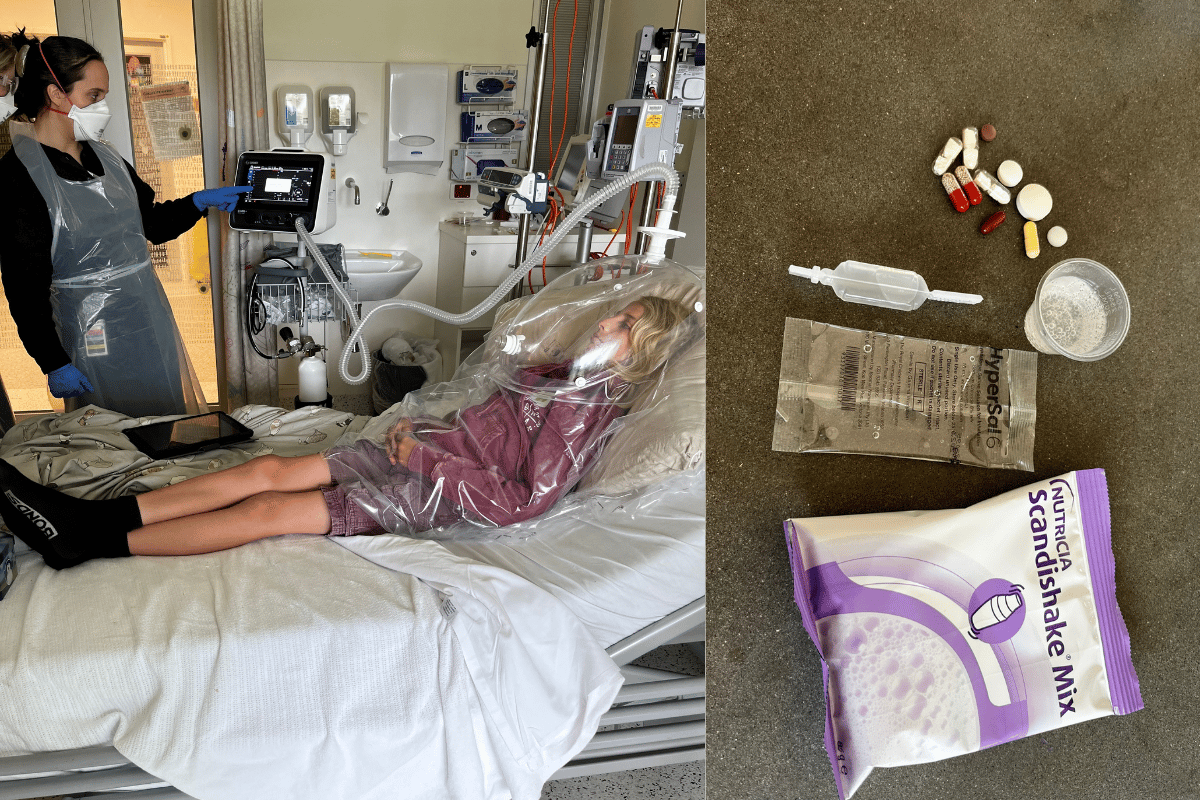
Watch: Daisy's cystic fibrosis treatment. Post continues below.
In Australia, one in 2,500 babies are born with the condition, and there is currently no cure. CF primarily affects the lungs and digestive system because of a malfunction in the exocrine system that's responsible for producing saliva, sweat, tears and mucus.