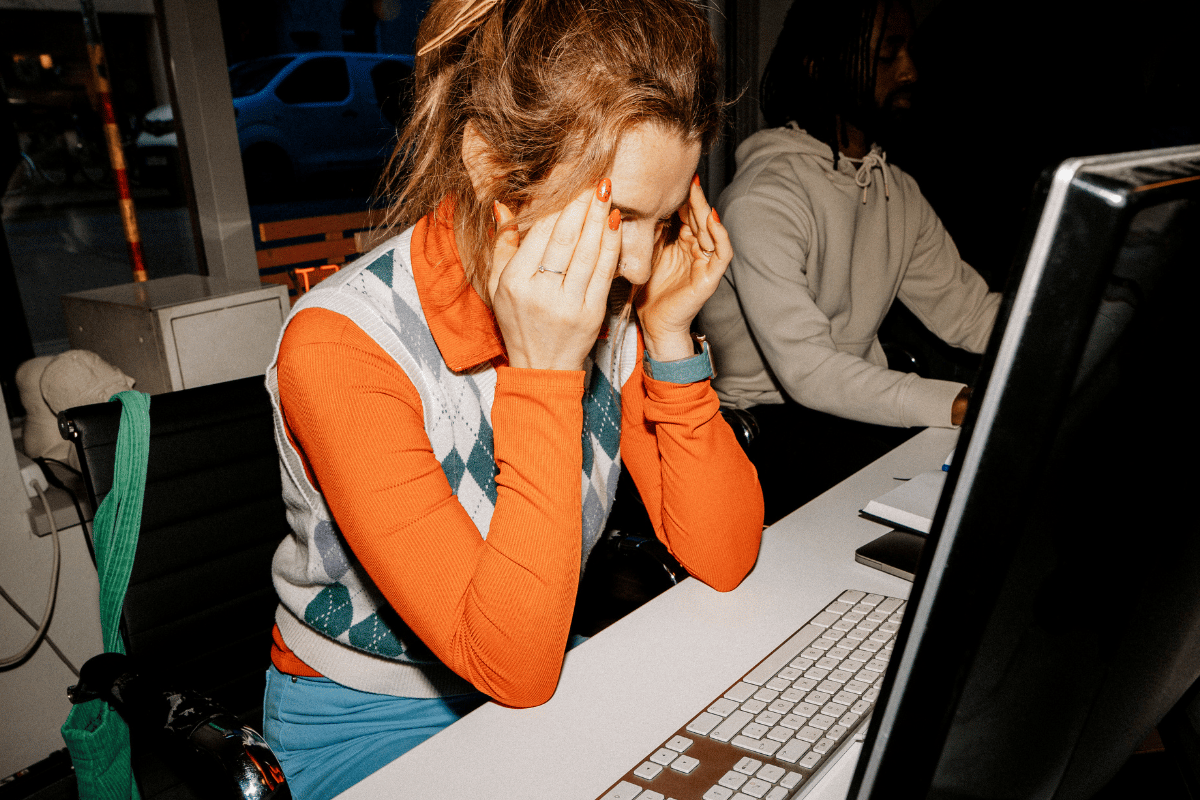
It's a frustrating experience I hear from so many people: you're exhausted, foggy, maybe losing hair, feeling flat or anxious – yet when you finally get your blood work checked, you're told everything is "normal."
Yet you don't feel like yourself.
This is especially common when it comes to iron. Iron deficiency isn't a simple black-and-white state.
Iron status is a spectrum that moves from depletion, to deficiency, to anaemia at the other.
Iron deficiency anaemia is the most significant stage, and it's sometimes only here that your blood test results will fall completely outside the "normal" range.
When you're in the earlier stages – depletion or deficiency – results are often skewed toward the lower end of normal, but not always technically outside it.
And that can leave you feeling confused, or even dismissed, if you know things aren't quite right but your tests look "fine" on paper.
Watch: Six ways to support your body and brain as you age. Post continues below.






























































































