Ever been to a doctor's appointment and felt kind of... rushed to get through everything? Like you have a list of questions in your head, but you're on the clock and there's just not enough time to cover everything? You're not alone.
A recent survey by The Royal Australian College of General Practitioners (RACGP) asked Australia’s GPs to vote on the biggest change needed in general practice to better serve Australian women.
According to the poll, 65 per cent of doctors said the number one most pressing change needed for women patients is to give them more time.
Watch: Dr Melissa Kang said she too turned to magazines for answers. Post continues below.
It was also found that GPs want better access to sexual and reproductive health services (14 per cent), enhanced preventative health screening programs (12 per cent), and more female GPs (seven per cent).
Listen: What is the “Uncool mental illness”? Mamamia Out Loud discusses. Post continues below.
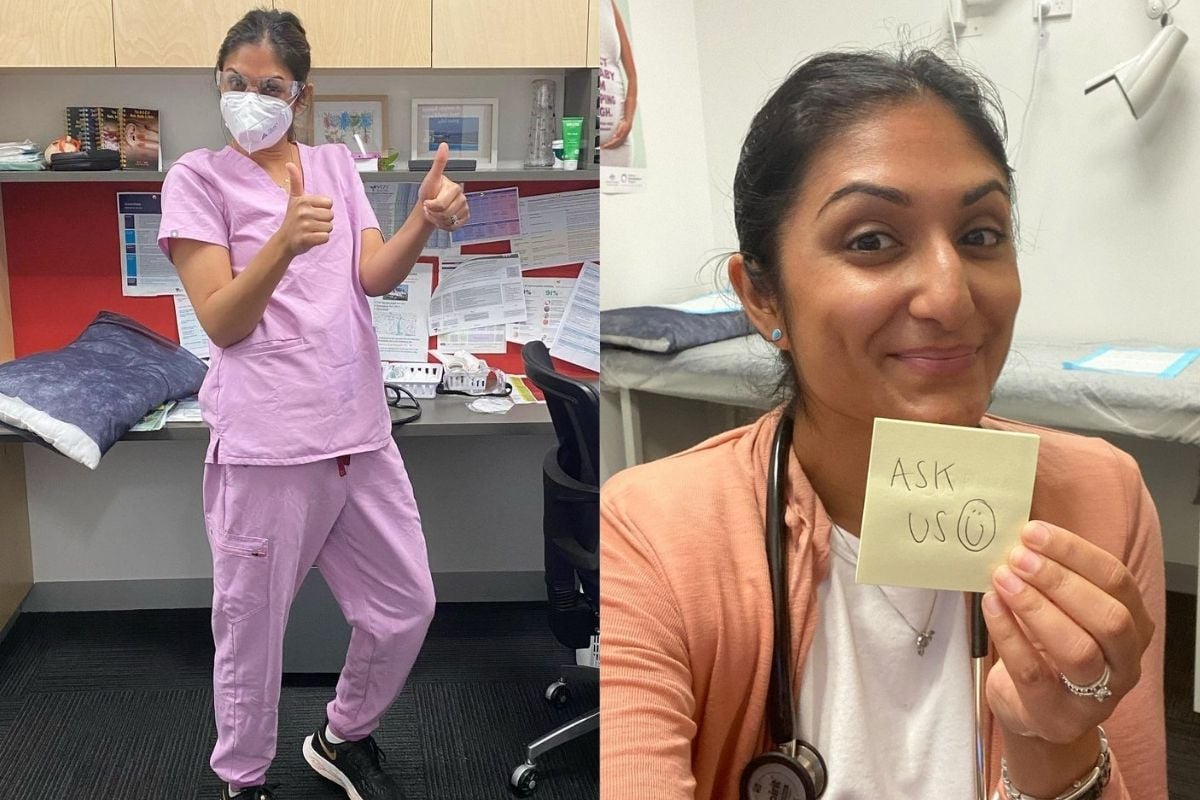
According to medical practitioner Dr Preeya Alexander, the push for longer consultations and changes within these healthcare services is not surprising.




























































































