This is a book extract from The Unexpected Journey by Emma Heming Willis, published by HarperCollins. You can buy it here.
If you want to support independent women's media, become a Mamamia subscriber. Get an all-access pass to everything we make, including exclusive podcasts, articles, videos and our exercise app, MOVE.
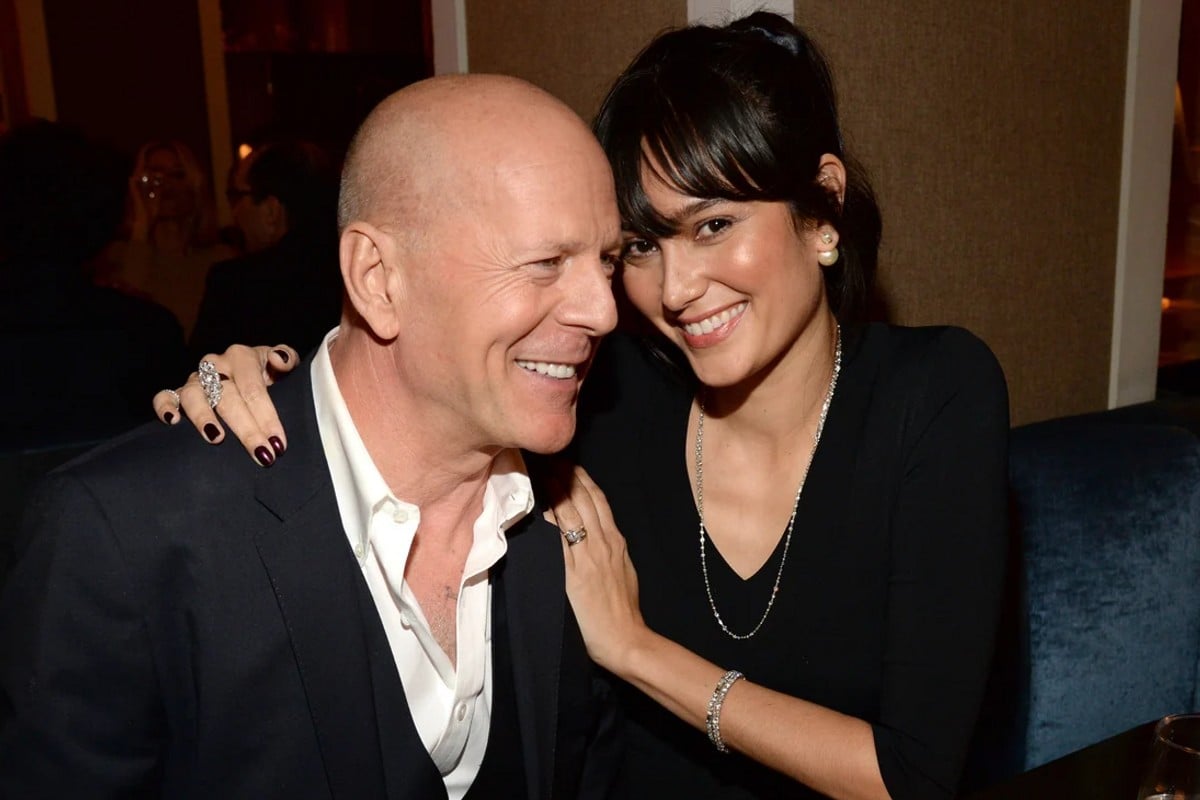
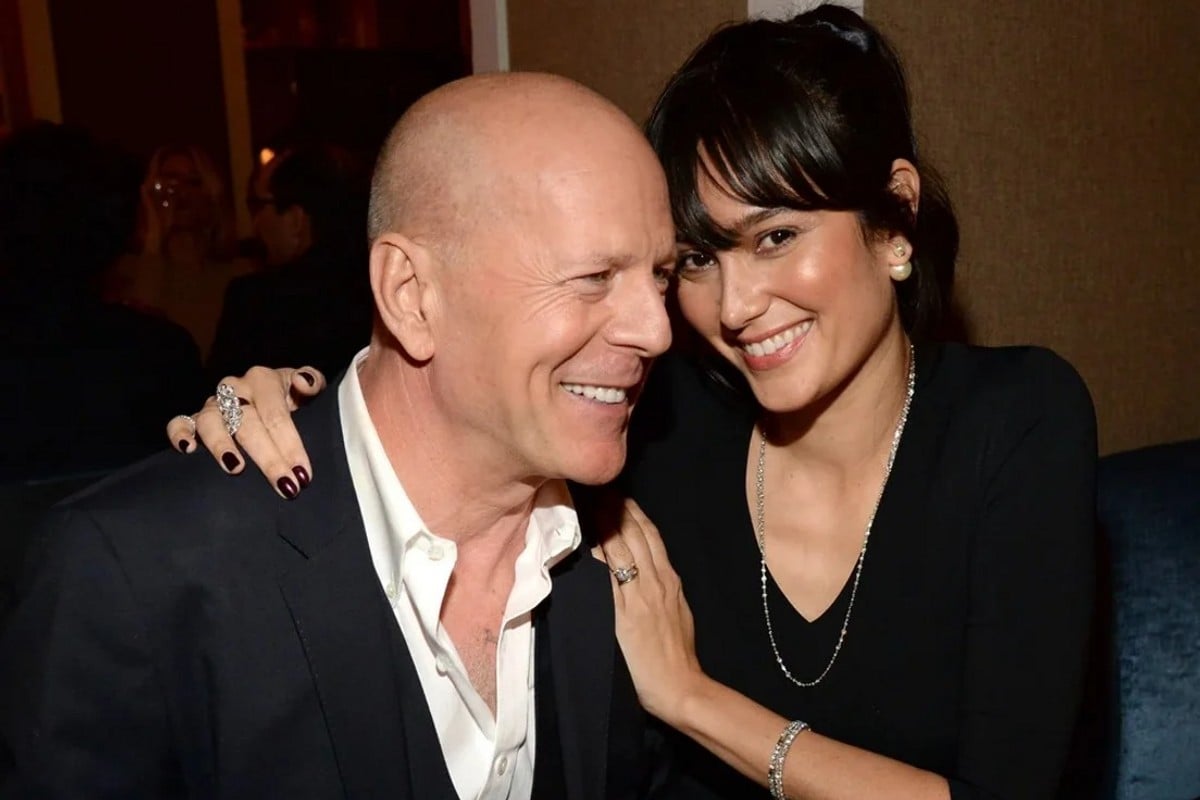
When I suspected something was "off" with Bruce but couldn't put my finger on what it was, I went through every possible explanation in my head.
Was there a problem in our marriage?
Was it Bruce's sleeping difficulties?
Maybe it was his hearing loss.
During the filming of the first Die Hard movie in the late '80s, there was a scene where he had to fire a gun underneath a table.
When it was shot, oddly, Bruce wasn't wearing any protective earplugs, and he lost a large percentage of his hearing in one ear.
When we first got together, this never posed a real problem.
Years later, however, I began to notice him sort of check out if we were at a dinner party or meal with the entire family.
Watch: Emma Heming Willis on World FTD Awareness Day. Post continues after video.