Stephen Duckett, Grattan Institute and Greg Moran, Grattan Institute
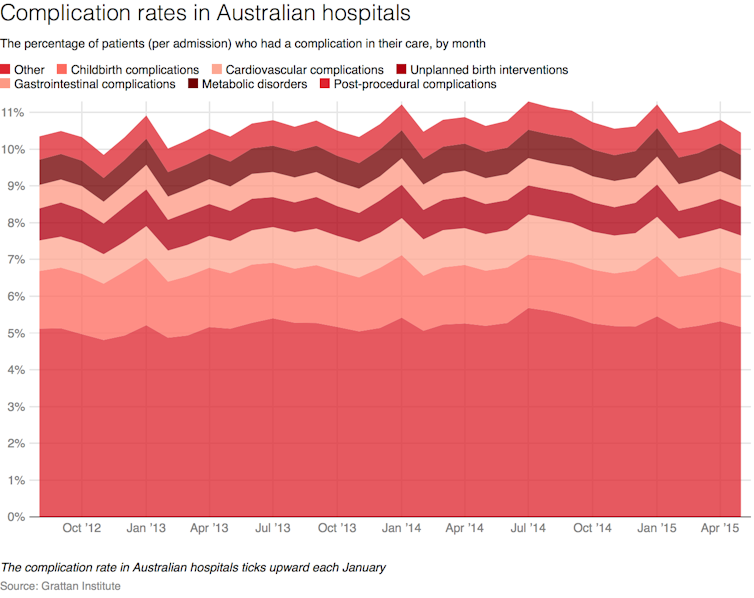
January is the quietest month in Australia. But for hospitals, which provide care 24/7/365, January is a time of big transition. And for patients, that means January is when things are more likely to go wrong.
More than 3,000 newly graduated doctors will enter the next phase of their training in January. New nurses and allied health professionals, such as physiotherapists and hospital pharmacists, also join the workforce in January.
These new staff fill the posts vacated by people one year ahead of them in the pipeline. Last year’s first-year-out doctor goes into his second year of training, and his predecessor goes into her third-year role or leaves the hospital to join a new workplace.
These new minds and hands, and the massive reshuffles of existing staff, disrupt hospitals. Old informal networks break down as new relationships are forged, and the less-experienced staff learn the hospital’s processes and expectations.
Read more: Reducing medical errors, one patient at a time
Not surprisingly, this staff disruption has an impact on patient care. Around the world, overblown descriptions of the changeover period as the “killing season” and of doctors’ first day in the UK as “Black Wednesday” have become part of medical folklore.
More sober studies of the “July Effect” (so named in the northern hemisphere) have indeed found evidence of worse patient outcomes during the changeover period.